Abstract
Background
Transforaminal lumbar interbody fusion (TLIF) with grafting and implant options like iliac crest bone graft (ICBG), recombinant bone morphogenetic protein (rhBMP), and polyetheretherketone (PEEK) cages have been reported to achieve extremely high fusion rates. Unfortunately, these options have also been frequently cited in the literature as causing postoperative morbidity and complications at a high cost. Knowing this, we sought to investigate TLIF using an acid-etched, roughened titanium cage that upregulates osteogenesis to see if similar fusion rates to those cited for ICBG, rhBMP, and PEEK cages could be safely achieved with minimal morbidity and complications.
Materials and methods
A radiographic fusion study of 82 patients who underwent TLIF using an acid-etched, roughened titanium cage with demineralized cancellous bone graft was conducted. Fusion was assessed and graded by an independent radiologist using computed tomography scan with sagittal and coronal reconstructions.
Results
Fusion rates at 6 months were 41 of 44 (93.2%) and at 12 months were 37 of 38 (97.4%). There were no radiographic device-related complications.
Conclusions
TLIF with an acid-etched, roughened titanium cage filled with a decalcified bone graft achieved similar fusion rates to historical controls using ICBG, rhBMP, and PEEK.
Introduction
Lower-back pain, radiculopathy, and other indications for lumbar fusion have been rising exponentially for years, making lumbar fusion one of the most common orthopedic surgical procedures. In fact, since the advent of lumbar cages in 1996, lumbar fusions have more than doubled, whereas hip replacement and knee arthroplasty—2 of the most common orthopedic surgical procedures—have risen at only a fraction of that amount.1
Research devoted to lumbar fusion has traditionally focused on fusion rates as primary outcome measures as considerable evidence has associated optimal bony fusion with clinical outcome and patient satisfaction.2, 3, 4 For example, Jiya et al.5 compared lumbar fusion rates and clinical outcome—measured with visual analog scale and clinical questionnaires—between interbody fusions using polyetheretherketone (PEEK) cages and poly-l-lactide-co-d,l-lactide cages and showed that patients with PEEK cages had significantly better fusion rates and clinical outcome scores than those with poly-l-lactide-co-d,l-lactide cages.
Lumbar fusion is one of the most commonly performed orthopedic surgical procedures. Advances in lumbar fusion due to innovations in spinal fusion implants and grafting options have been dramatic—leading to improvements in the rates of successful fusions. Early studies showed posterolateral fusions with iliac crest bone graft (ICBG) to have fusion rates ranging from 73%–90%.6, 7, 8, 9 Later studies investigating anterior lumbar interbody fusion with alternatives to ICBG, such as calcium sulfate and PEEK cages with local autograft, demonstrated fusion rates exceeding 90%.5, 9 More recently, investigators have reported fusion rates of 95%–100% for anterior lumbar interbody fusion performed with recombinant human bone morphogenetic protein (rhBMP) and PEEK cage implants.7, 8 Finally, studies reporting on transforaminal interbody fusion approach (TLIF) and posterior lumbar interbody fusion (PLIF), a recent interbody fusion procedural advance—with and without rhBMP, have shown fusion rates nearing 100%.7, 10, 11, 12, 13, 14 Schwender et al.14 reported fusions in all 45 patients who underwent TLIF with PEEK cage and rhBMP, while Rihn et al.7 reported fusions in 95.8% of patients.
In addition to advances in grafting options and implant technology, the surgical techniques for lumbar fusion have evolved considerably. Currently, interbody fusions such as TLIF and PLIF have gained popularity, as they can achieve higher fusion rates than traditional posterolateral surgical approaches.3, 13, 14, 15, 16, 17, 18, 19, 20, 21 Both TLIF and PLIF achieve interbody fusion from a posterior approach and lead to wider areas of intervertebral bone-to-graft contact than posterolateral fusion, while restoring disc space height, lumbar lordosis, and coronal-sagittal balance of the spine.17 TLIF has surpassed PLIF in popularity as TLIF—owing to its more lateral exposure of the interspace—allows preservation of the posterior longitudinal ligament complex as well as other supporting bony and ligamentous structures, which are often compromised in PLIF.13, 14, 16, 21 In addition, minimal neural retraction or epidural dissection is required in TLIF, as compared with PLIF.3, 14, 21
Although the innovations in spinal fusion technology have improved fusion rates, there is concern that these achievements come at the cost of greater patient morbidity and dissatisfaction. Firstly, the morbidity associated with ICBG—largely owing to pseudarthrosis and donor site complications—has been the impetus for use and development of safer graft options.2, 9 Secondly, PEEK cages frequently require revision surgery owing to fibrous union, subsidence, posterior migration, and impingement on the thecal sac.18, 22, 23 Lastly, lumbar fusion with rhBMP has consistently led to reports of osteolysis, postoperative radiculitis, ectopic bone formation, and other serious complications requiring revision surgery.3, 7, 14, 15, 16, 21, 22, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33
Appreciating these complication rates for lumbar fusion utilizing ICBG, rhBMP, and PEEK cages, this study sought to determine whether TLIF using an acid-etched, roughened titanium cage that upregulates osteogenesis could safely achieve lumbar fusion rates similar to those cited for the aforementioned grafting and implant options at 6 and 12 months after the index procedure.
Clinical materials and methods
Study design
The authors selected 86 consecutive patients who underwent TLIF with a titanium cage and biological demineralized bone graft. These patients were divided into 2 separate cohorts—according to time after surgery—6 and 12 months. A period of 6 months was chosen as this is a common short-term follow-up period used in comparable TLIF studies2, 12; 12 months was chosen because it is widely accepted as the cutoff when patients can be considered to have achieved fusion or not. Indications for surgery included diagnoses of spondylolisthesis, recurrent herniated disc, degenerative disc disease, or spinal stenosis. All patients underwent TLIF using the same implants and allograft (Titan Spine's Endoskeleton TT with Bacterin's OsteoSponge). Clinical results are reported for 44 patients at 6 months and 38 patients at 12 months.
Surgical procedure
A standard posterior approach with complete laminectomy and medial facetectomy, along with decompression if indicated, was performed. After decompression, standard pedicle screw instrumentation was utilized. Before insertion of the screws, 3 mL of bone marrow aspirate (BMA) was aspirated from the vertebral body. The BMA was used to reconstitute the OsteoSponge allograft.
A standard annulotomy was performed, and starting incrementally from 7 up to 14 mm, serial dilators were used to distract the interspace. In addition, the dilators served to clean the disc material and meticulously prepare the disc space. Once the disc space was prepared, an appropriate size trial was inserted and fluoroscopy was obtained to verify position and correct sizing.
A strip of OsteoSponge was placed as anteriorly as possible in the disc space, followed by placement of OsteoSponge into the cage, with the cage inserted obliquely and turned to sit in parallel to the endplates as anteriorly as possible in the intervertebral space. The posterior aspect of the interspace was then packed with ground autologous bone harvested during the laminectomy. Finally, the pedicle screws were compressed and locked.
Titan Endoskeleton TT and OsteoSponge/BMA
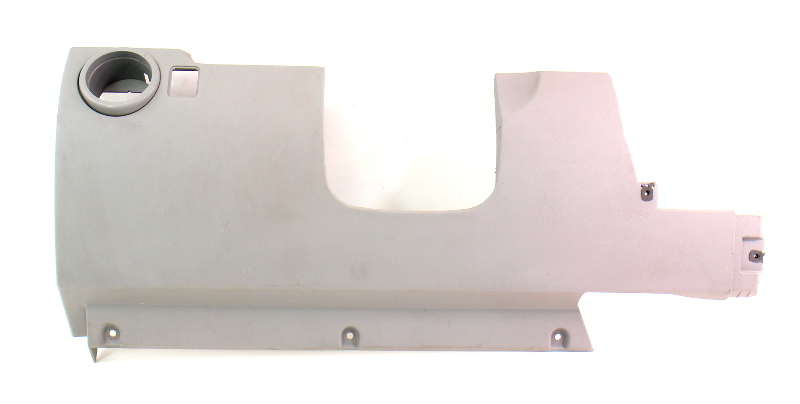
The Endoskeleton TT (Fig. 1) is a titanium alloy interbody device designed to aid in the fusion of 1 or 2 contiguous levels between L2 and S1 through a TLIF. This device features a surface treatment that includes a combination of textures at the macrolevel and the microlevel. In vitro studies indicate that this surface may upregulate significantly critical bone growth factors necessary for fusion.34
![View full-size image.]()
Fig. 1.
(A) Titan Spine's Endoskeleton TT. (B) Lateral view of Titan Spine's Endoskeleton TT (C) Cross-sectional view of Titan Spine's Endoskeleton TT. (D) Fluoroscopy of Titan Spine's Endoskeleton TT. (E) CT-scan coronal and sagittal images.
The OsteoSponge allograft (Bacterin International, Belgrade, Montana) is a nonstructural bone void filler composed of human demineralized cancellous bone, with no additional carrier materials.38 When hydrated with BMA, the graft becomes compressible, exhibits shape memory, and can be compressed and inserted into an interbody device where it expands to enhance connectivity at the graft-bone interface. OsteoSponge maintains the porosity of cancellous bone (Fig. 2), allowing it to serve as a scaffold to facilitate bony fusion.
![View full-size image.]()
Fig. 2.
Microscopic CT image of the OsteoSponge allograft illustrating the interconnected pore structure.
Postoperative imaging protocol
Noncontrast fine-cut computed tomography (CT) scans with axial, sagittal, and coronal reconstruction were performed on all patients. The images were reviewed on an InteleViewer PACs workstation by a fellowship trained and Certificate of Added Qualification–certified neuroradiologist who was independent and blinded to whether the scan was performed at 6 or 12 months postoperatively.
Evaluation was performed using a simple, reproducible fusion grading system devised by the authors (Table 1). A grade III or IV was deemed with confidence to reflect a satisfactory degree of solid bony fusion.
Table 1. Grading system
| Points | ||
|---|---|---|
| Spacer margins | 0 | Any evidence of subsidence or lucency around the cage |
| 1 | Tightly marginated with both endplates without bone resorption or subsidence | |
| Bone within cage | 0 | Lucency within cage similar to nonossified disc |
| 1 | Increased density within spacer beyond that of nonossified disc space suggestive of trabecular bone | |
| Bone bridge between endplates | 0 | No bony bridging between endplates |
| 1 | < 0.5 cm bridge on either sagittal or coronal reconstruction | |
| 2 | ≥ 0.5 cm bridge on either sagittal or coronal reconstruction |
Maximum score = 4.
Results
Patient characteristics
Overall, 42 patients followed up for 6 months after TLIF with the titanium cage were included in the 6-month follow-up arm, while 34 patients followed up for 12 months after TLIF with the titanium cage were included in the 12-month follow-up arm. Patient demographics are summarized in Table 2.
Table 2. Patient demographics
| Six months | Twelve months | |
|---|---|---|
| 44 | 38 | |
| Average age, year | 51.0 | 48.0 |
| Male:female | 21:23 | 15:23 |
| Operative levels | ||
| L2-L3 | 0 | 0 |
| L3-L4 | 6 | 4 |
| L4-L5 | 21 | 16 |
| L5-S1 | 17 | 18 |
Fusion rate
Fusion rates are summarized in Table 3. Of the 44 patients in the 6-month follow-up arm, 31 (70.5%) had a fusion grade of IV, 10 (22.7%) had a grade of III, 2 (4.5%) had a grade of II, and 1 (2.3%) had a grade of I. The total fusion rate for the 6-month follow-up arm—rate of patients with grade III or higher—was 93.2%.
Table 3. Fusion rates
| Fusion | ||||
|---|---|---|---|---|
| Grade | n | % | Fusion (Y/N) | Fusion % |
| Six-month cohort | ||||
| Grade I | 1 | 2.3 | N | 0 |
| Grade II | 2 | 4.5 | N | 0 |
| Grade III | 10 | 22.7 | Y | 22.7 |
| Grade IV | 31 | 70.5 | Y | 70.5 |
| Total | 44 | 100 | N/A | 93.2 |
| Percentage Y (fusion rate) | 93.2 | |||
|
| ||||
| Twelve-month cohort | ||||
| Grade I | 1 | 2.6 | N | 0 |
| Grade II | 0 | 0 | N | 0 |
| Grade III | 9 | 23.7 | Y | 23.7 |
| Grade IV | 28 | 73.7 | Y | 73.7 |
| Total | 38 | 100 | N/A | 97.4 |
| Percentage Y (fusion rate) | 97.4 | |||
Y = Defined as fusion; N = Defined as not a fusion; N/A = Not appropriate.
Of the 38 patients in the 12-month follow-up arm, 28 (73.7%) had a fusion grade of IV, 9 (23.7%) had a grade of III, 0 (0%) had a grade of II, and 1 (2.6%) had a grade of I. The total fusion rate for the 12-month follow-up arm—rate of patients with grade III or higher—was 97.4%.
Complications
None of the patients in either arm experienced implant-related major complications from the procedure such as dural tear, osteolysis, postoperative radiculopathy, infection, subsidence of implant, or dislodgement of implant.
Discussion
There have been numerous advances and innovations in lumbar fusion over the last 20 years, with the goal of optimizing fusion rates and minimizing patient morbidity. Early studies investigating lumbar fusion with ICBG showed high fusion rates, with some reporting rates greater than 90%.27 Additional studies investigating alternatives to ICBG have reported equally favorable or improved fusion rates. Mummaneni et al.35 reported fusion in 20 of 21 patients undergoing TLIF with rhBMP and local bone autograft implanted in PEEK cages, while Villavicencio et al.36 reported a 100% fusion rate after 10 months using similar fusion constructs with rhBMP.2, 7
Significant patient morbidity has been reported in patients undergoing traditional lumbar fusion procedures. Rihn et al.7 showed that as many as 60% of patients undergoing ICBG experience long-term, persistent donor site pain, while 2%–5% of patients develop wound complications that require reoperation. Vaidya et al.31 reported that the use of rhBMP in TLIF led to cage migration in 33% of patients, with reoperation required in all the patients because of neurological compromise. McClellan et al.37 reported osteolysis and bone resorption in 69% of the operated levels for patients undergoing TLIF with rhBMP, while Rihn et al.28 found 14% of patients undergoing TLIF with rhBMP to have postoperative radiculitis.29 When considering these and other reports on TLIF with rhBMP, it is important to emphasize that—in addition to its concerning complication rate—rhBMP carries high financial costs.
The reports of complications and morbidity associated with ICBG, rhBMP, and PEEK cages—combined with rhBMPs high cost—inspired us to investigate TLIF utilizing an acid-etched, roughened titanium cage to see if fusion rates achieved with this device compared favorably to the rates cited for TLIF with other commonly used graft options and implants. Our results show that TLIF using this titanium cage can safely achieve solid bony fusion in 93.2% and 97.4% of patients followed up for 6 months and 12 months, respectively.
The acid-etched, roughened titanium cage used in this study contains a treatment to create a textured surface at the macrolevel, microlevel, and cellular level, which provides an enhanced bone growth response. Common interbody device materials such as PEEK primarily cause stem cells to flatten on the surface of the implant and differentiate into fibroblasts—cells responsible for fibrous union—whereas, the surface of this titanium cage promotes differentiation into osteoblasts—cells crucial for osteogenesis—that lead to solid bony union. One pivotal study by Olivares-Navarrete et al.34 in The Spine Journal showed that the cellular process set in motion by the surface technology induces the body to produce and regulate its own BMPs—specifically BMP-2, BMP-4, and BMP-7—and other critical bone growth and angiogenic factors at the key stages of the fusion process. This supports new bone growth and negates the need for costly and potentially hazardous BMP supplementation. In addition to shifting pluripotent cell differentiation toward osteogenic cells and away from fibrogenic cells, this device allows for visualization of fusion on CT and magnetic resonance imaging, which is different from traditional cylindrical titanium cages that cause significant scatter during imaging, which makes assessment of fusion difficult.17
The OsteoSponge is a grafting option used in conjunction with structural interbody devices for spinal fusion. Owing to its malleable properties, it can be inserted into a variety of void sizes and expands to maintain direct contact with the vertebral endplates. This property—combined with the osteoconductive structure of cancellous demineralized bone matrix—makes this graft material suitable for primary fusion applications.39
The fusion rates achieved in this study are similar to the rates cited in previous lumbar fusion studies. Kasliwal et al.2 reported a fusion rate of 67.5% in patients—with a mean follow-up of 22 months (range 12–62 months)—undergoing TLIF with local autograft and PEEK cages. Helgeson et al.3 showed a fusion rate of 83% in patients 2 years after undergoing TLIF with rhBMP and PEEK cages. Dimar et al.6 published fusion rates of 73% and 88% for patients 2 years after undergoing lumbar fusion with ICBG and rhBMP, respectively. Finally, a meta-analysis by Wu et al.21—with a mean follow-up of 26.6 months (range 6–46 months)—showed TLIF fusion rates to be 90.9%–94.8%, depending on the type of graft and surgical exposure.
Limitations of the study
The first limitation of this study that requires mentioning is the lack of a control group as all the patients in both arms of the study underwent TLIF with the same titanium cage. This prevents direct efficacy and safety comparisons between our implant and procedure and other procedures that have been previously cited.
Another limitation of this study is that we used a unique classification system and definition of fusion that has not been previously described. It is important to note that our study's fusion classification system and definition was made before beginning the study by an experienced radiologist who was blinded to the study design. It is also important to emphasize that currently, there is no universally accepted fusion grading system or definition, and this has led to enormous variability in the fusion classification systems and definitions reported in the literature.5, 21 For example, Chen et al. used X-ray and not CT and defined fusion as conclusive evidence of continuous intertransverse bony bridging at all levels. Arnold et al. used anteroposterior, lateral, and flexion-extension (F-E) radiographs and defined fusion parameters as less than 12% anterior/posterior translation on F-E radiographs, less than 5° rotation (Cobb angle) between F-E radiographs, maintenance of disc height, and evidence of bridging trabecular bone.18 However, our system is strikingly similar to classification systems and definitions cited in previous studies and used CT evaluation, which is important as CT has been shown to be more accurate and effective than X-ray at delineating fusion.2, 6, 8, 13 X-ray, being a less accurate diagnostic tool for assessing fusion, has been shown to overestimate fusion rates, and this may partially explain the 100% fusion rate reported by Schwender et al. and other studies utilizing X-ray instead of CT.2
Conclusion
Transforaminal lumbar interbody fusion surgery is a common surgical procedure, while ICBG, rhBMP, and PEEK cages are common graft options and implants. Our study sought to determine whether TLIF using an acid-etched, roughened titanium cage could safely achieve similar fusion rates as TLIF using the aforementioned graft and implant options. The findings in this study demonstrate that 93.2% of patients achieved fusion with no device or approach-related complications after 6 months, and a fusion rate of 97.4% was achieved at 12 months. These fusion rates compare equally well with other lumbar fusion studies cited in the literature. Additional research may be useful to better elucidate the optimal combination of implant and biological graft material to achieve the most reliable and rapid fusion outcome.
References
- Deyo RA, et al. United States trends in lumbar fusion surgery for degenerative conditions. Spine. 2005;30(12):1441–1445
- Kasliwal M, Deutsch H. Clinical and radiographic outcomes using local bone shavings as autograft in minimally invasive transforaminal lumbar interbody fusion: Technical note. World Neurosurg. 2012;78(1-2):185–190
- Helgeson MD, et al. Adjacent vertebral body osteolysis with bone morphogenetic protein use in transforaminal lumbar interbody fusion. Spine J. 2011;11(6):507–510
- Mulconrey DS, et al. Bone morphogenetic protein (RhBMP-2) as a substitute for iliac crest bone graft in multilevel adult spinal deformity surgery: Minimum two-year evaluation of fusion. Spine. 2008;33(20):2153–2159
- Jiya TU, et al. Posterior lumbar interbody fusion using non resorbable poly-ether-ether-ketone versus resorbable poly-l-lactide-co-d, l-lactide fusion devices. Clinical outcome at a minimum of 2-year follow-up. Eur Spine J. 2011;20(4):618–622
- Dimar JR, et al. Clinical outcomes and fusion success at 2 years of single-level instrumented posterolateral fusions with recombinant human bone morphogenetic protein-2/compression resistant matrix versus iliac crest bone graft. Spine. 2006;31(22):2534–2539
- Rihn JA, Kirkpatrick K, Albert TJ. Graft options in posterolateral and posterior interbody lumbar fusion. Spine. 2010;35(17):1629–1639
- Glassman SD, et al. Complications and concerns with osteobiologics for spine fusion in clinical practice. Spine. 2010;35(17):1621–1628
- Chen WJ, et al. The fusion rate of calcium sulfate with local autograft bone compared with autologous iliac bone graft for instrumented short-segment spinal fusion. Spine. 2005;30(20):2293–2297
- McKay WF, Peckham SM, Badura JM. A comprehensive clinical review of recombinant human bone morphogenetic protein-2 (INFUSE® Bone Graft). Int Orthop. 2007;31(6):729–734
- Carter JD, et al. Clinical and radiographic assessment of transforaminal lumbar interbody fusion using HEALOS collagen-hydroxyapatite sponge with Autologous bone marrow aspirate. Spine J. 2009;9(6):434–438
- Kawaguchi S, et al. Fusion status and clinical outcomes at one year and two years of instrumented, local bone transforaminal lumbar interbody fusion. J Spine. 2012;1(103):2
- Rouben D, Casnellie M, Michael F. Long-term durability of minimal invasive posterior transforaminal lumbar interbody fusion: A clinical and radiographic follow-up. J Spinal Disord Tech. 2011;24(5):288–296
- Schwender JD, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): Technical feasibility and initial results. J Spinal Disord Tech. 2005;18:S1–S6
- Knox JB, Dai JM, Orchowski J. Osteolysis in transforaminal lumbar interbody fusion with bone morphogenetic protein-2. Spine. 2011;36(8):672
- Owens K, et al. Perioperative complications with rhBMP-2 in transforaminal lumbar interbody fusion. Eur Spine J. 2011;20(4):612–617
- Cole CD, et al. Comparison of low back fusion techniques: Transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody fusion (PLIF) approaches. Curr Rev Musculoskelet Med. 2009;2(2):118–126
- Arnold PM, et al. Clinical outcomes of lumbar degenerative disc disease treated with posterior lumbar interbody fusion allograft spacer: A prospective, multicenter trial with 2-year follow-up. Am J Orthop. 2009;38(7):115–122
- Peng CW, et al. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine. 2009;34(13):1385–1389
- Schizas C, et al. Minimally invasive versus open transforaminal lumbar interbody fusion: Evaluating initial experience. Int Orthop. 2009;33(6):1683–1688
- Wu RH, Fraser JF, Roger H. Minimal access versus open transforaminal lumbar interbody fusion: Meta-analysis of fusion rates. Spine. 2010;35(26):2273
- Duncan JW, Bailey RA. An analysis of fusion cage migration in unilateral and bilateral fixation with transforaminal lumbar interbody fusion. Eur Spine J. 2012;22(2):1–7
- Kim PD, Baron EM, Levesque M. Extrusion of expandable stacked interbody device for lumbar fusion: Case report of a complication. Spine. 2012;37(18):E1155–E1158
- Anderson CL, Whitaker M. Heterotopic ossification associated with recombinant human bone morphogenetic protein-2 (Infuse) in posterolateral lumbar spine fusion: A case report. Spine. 2012;37(8):E502
- Carragee EJ, et al. Retrograde ejaculation after anterior lumbar interbody fusion using rhBMP-2: A cohort controlled study. Spine J. 2011;11(6):511–516
- Crawford CH, et al. Perioperative complications of recombinant human bone morphogenetic protein-2 on an absorbable collagen sponge versus iliac crest bone graft for posterior cervical arthrodesis. Spine. 2009;34(13):1390
- Glassman SD, et al. The efficacy of rhBMP-2 for posterolateral lumbar fusion in smokers. Spine. 2007;32(15):1693–1698
- Rihn JA, et al. The use of RhBMP-2 in single-level transforaminal lumbar interbody fusion: A clinical and radiographic analysis. Eur Spine J. 2009;18(11):1629–1636
- Nasca RJ. Osteolysis in lumbar interbody fusions: The role of recombinant human bone morphogenetic protein-2 (rhBMP-2). Duke Orthop J. 2011;2(1):50–54
- Smoljanovic T, Bojanic I, Delimar D. Adverse effects of posterior lumbar interbody fusion using rhBMP-2. Eur Spine J. 2009;18(6):920–923
- Vaidya R, et al. Complications in the use of rhBMP-2 in PEEK cages for interbody spinal fusions. J Spinal Disord Tech. 2008;21(8):557–562
- Williams BJ, et al. Does bone morphogenetic protein increase the incidence of perioperative complicationsin spinal fusion? A comparison of 55,862 cases of spinal fusion with and without bone morphogenetic protein. Spine. 2011;36(20):1685–1691
- Woo EJ. Recombinant human bone morphogenetic protein 2: Adverse events reported to the Manufacturer and User Facility Device Experience database. Spine J. 2012;12(10):894–899
- Olivares-Navarrete R, et al. Osteoblasts exhibit a more differentiated phenotype and increased bone morphogenetic protein production on titanium alloy substrates than on poly-ether-ether-ketone. Spine J. 2012;12(3):265–272
- Mummaneni PV, Pan J, Haid RW, et al. Contribution of recombinant human bone morphogenetic protein-2 to the rapid creation of interbody fusion when used in transforaminal lumbar interbody fusion: A preliminary report. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1:19–23
- Villavicencio AT, Burneikiene S, Nelson EL, et al. Safety of transforaminal lumbar interbody fusion and intervertebral recombinant human bone morphogenetic protein-2. J Neurosurg Spine. 2005;3:436–443
- McClellan JW, Mulconrey DS, Forbes RJ, Fullmer N. Vertebral bone resorption after transforaminal lumbar interbody fusion with bone morphogenetic protein (rhBMP-2). J Spinal Disord Tech. 2006;19:483–486
- Miller LE, Jacofsky DJ, Kirker KR. Rationale, characteristics, and clinical performance of the OsteoSponge®: A novel allograft for treatment of osseous defects. Orthop Res Rev. 2012;4:9–17
- Brigido SA, Bleazey ST, Protzman NM, et al. A retrospective analysis evaluating allogeneic cancellous bone sponge for foot and ankle arthrodesis. J Foot Ankle Surg. 2013;52:28–31
Corresponding author: Gerad Girasole, MD, OSM 888 White plains Road, Trumbull, CT 06611; Tel.: +1-203-268-2882.